Grief is a deeply personal journey—an emotional, psychological, and even physical experience. But what many people don’t realize is that grief is also a physiological process, one that is closely tied to our hormones. For women, whose hormonal cycles are already complex and dynamic, grief can feel especially intense, unpredictable, and at times overwhelming. Understanding how hormones influence the grieving process can provide both clarity and comfort during one of life’s most difficult times.
The Hormone-Grief Connection
Hormones are powerful chemical messengers that regulate everything from mood to metabolism. In women, fluctuations in estrogen, progesterone, cortisol, and oxytocin can shape how we emotionally and physically process loss. Let’s explore how each plays a role:
1. Estrogen and Emotional Sensitivity
Estrogen is often linked to mood regulation and emotional sensitivity. When estrogen levels are high (as during ovulation), many women report feeling more emotionally responsive or even raw. Conversely, during low-estrogen phases—like menstruation or perimenopause—mood dips are common. Grieving during these times can intensify feelings of sadness, isolation, and hopelessness.
In fact, research suggests that women are more likely than men to experience mood disorders in response to grief, partly due to these hormonal vulnerabilities. This doesn’t mean women are “too emotional”—it means their bodies are literally wired to feel loss on a cellular level.
2. Progesterone and Fatigue
Often called the “calming hormone,” progesterone can have a sedating effect. After a loss, women may feel more tired or emotionally numb when progesterone is dominant, like in the luteal phase of the menstrual cycle. This hormonal dip can mask or intensify grief depending on the timing, leading to a confusing rollercoaster of emotions.
Progesterone also interacts with GABA receptors in the brain—the same receptors targeted by anti-anxiety medications. This might explain why some women feel emotionally dulled or disconnected during parts of their cycle, especially while grieving.
3. Cortisol: The Stress Hormone
Grief is a form of psychological trauma, and the body reacts accordingly. Cortisol, the primary stress hormone, often surges after a significant loss. In the short term, this helps the body cope with acute stress. But over time, high cortisol levels can lead to sleep disturbances, anxiety, brain fog, and even immune suppression—all of which complicate the grieving process.
Women are especially susceptible to chronic stress responses, and when combined with hormonal changes due to menstruation, menopause, or postpartum shifts, the results can be physically and emotionally draining.
4. Oxytocin: The Bonding Hormone
Oxytocin is released during connection, intimacy, and caregiving. It’s the hormone that fosters bonding, especially in mothers and caregivers. When we lose someone we love, oxytocin levels can plummet, contributing to a sense of emptiness or longing. For women who have lost a child, partner, or someone they cared for deeply, the absence of oxytocin-related bonding can be a source of profound grief that goes beyond words.
Special Considerations: Pregnancy, Postpartum, and Menopause
Certain life stages can amplify the hormonal dimensions of grief:
During pregnancy, grief can feel intensified as hormonal surges amplify emotional responses. There’s also a strong protective instinct that can make loss feel even more threatening or destabilizing. Postpartum grief—whether from the loss of a pregnancy, infant, or another loved one—collides with already dramatic hormonal shifts, increasing the risk of depression or anxiety. Menopausal women may experience grief differently, as declining estrogen and progesterone levels can affect emotional regulation and memory, sometimes making it harder to process or even remember aspects of their grief clearly.
What You Can Do
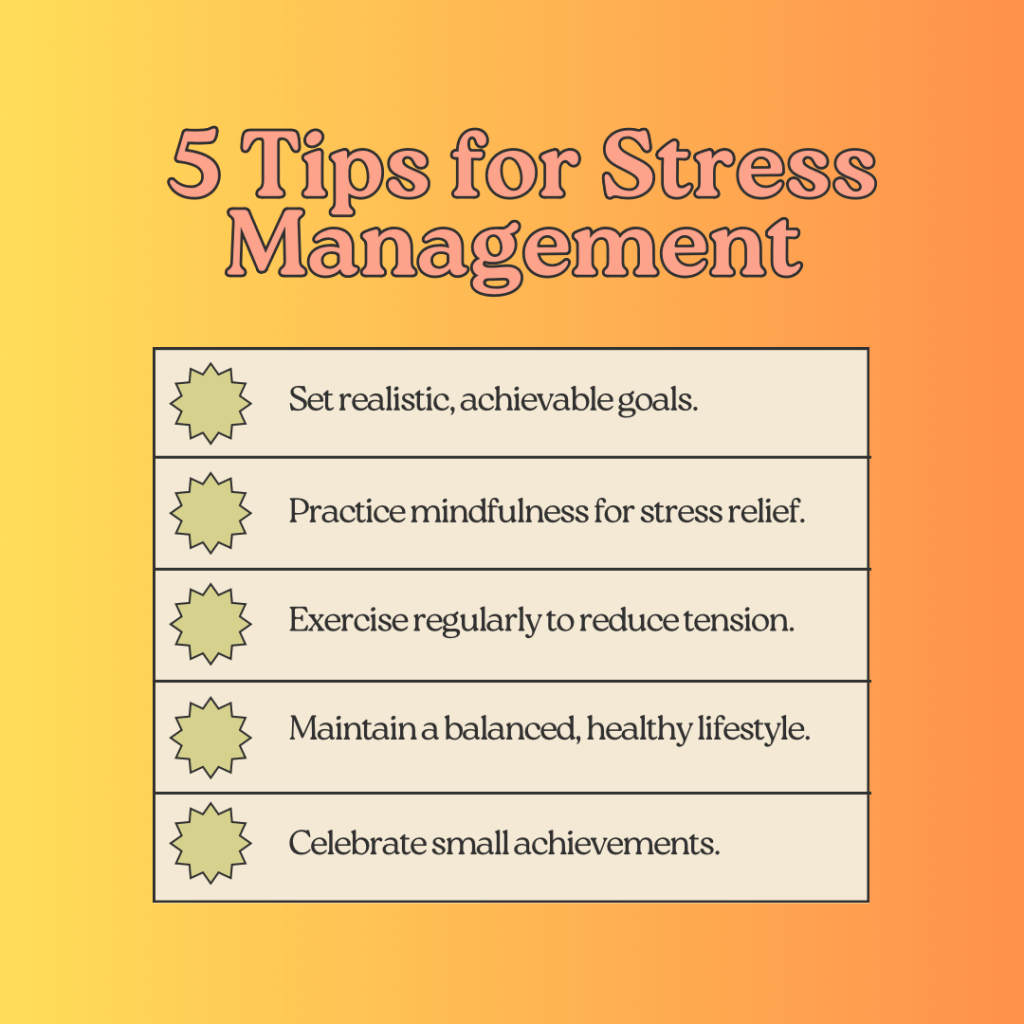
Understanding that hormones play a significant role in grief doesn’t take away the pain—but it can help women give themselves more grace. Here are a few gentle practices that may help:
Track your cycle and note how different phases affect your grief responses. Prioritize rest and nutrition, especially during low-hormone phases or high-stress times. Seek connection, even when it feels difficult. Oxytocin needs human contact to flow. Talk to a professional—grief counselors, therapists, and even hormone specialists can provide tools that honor both the emotional and physiological dimensions of loss.
In Closing
Grief isn’t just in your head—it’s in your hormones, your bones, your skin. For women, the grieving process is not linear, and it is often magnified by the natural rhythms of the body. By understanding and honoring how hormones shape our emotional worlds, we can grieve more mindfully and compassionately.
You’re not broken. You’re human—and you’re healing in your own, hormonally influenced way.
Leave a comment